Listen up, friends. If you're reading this, chances are you're dealing with something that's been bugging you—literally. UTIs that won’t go away even after two rounds of antibiotics are a real pain in the you-know-what. And trust me, no one wants to deal with this kind of inconvenience. So, let's dive right in. Why does this happen? What can you do about it? And most importantly, how do you stop it from ruining your life?
We all know urinary tract infections (UTIs) are no joke. They sneak up on you when you least expect it, causing burning sensations, frequent trips to the bathroom, and sometimes even a fever. But what happens when antibiotics, the superhero of the medical world, just don’t cut it? That’s the situation we’re tackling today. If your UTI won’t go away after two rounds of antibiotics, you’re not alone. Thousands of people face this issue every year, and it’s time to get some answers.
This article is here to help. We’ll break down the reasons why UTIs might persist, explore alternative treatments, and give you actionable advice to take back control of your health. So, grab a cup of tea, sit back, and let’s figure this out together.
Read also:Josh Winterhalt Unveiling The Journey Of A Rising Star
Table of Contents
- Understanding UTI: The Basics
- Why Does UTI Persist After Antibiotics?
- Types of UTIs and Their Complexity
- Antibiotic Resistance: A Growing Concern
- The Diagnosis Process: What to Expect
- Alternative Treatments for Persistent UTIs
- Lifestyle Changes to Prevent Recurrence
- Home Remedies That Might Help
- When to See a Doctor
- Final Thoughts: Taking Control of Your Health
Understanding UTI: The Basics
Before we dive into the nitty-gritty, let’s get our basics straight. UTIs, or urinary tract infections, are infections that affect any part of your urinary system, including your bladder, kidneys, ureters, and urethra. Most UTIs involve the lower urinary tract—the bladder and the urethra. Symptoms can range from mild discomfort to severe pain, and they often include:
- A strong, persistent urge to urinate
- A burning sensation when urinating
- Passing small amounts of urine frequently
- Cloudy or strong-smelling urine
- Blood in the urine
Now, here’s the kicker. UTIs are usually caused by bacteria, most commonly E. coli, which normally live in your digestive tract. When these bacteria find their way into your urinary tract, they can multiply and cause an infection. And while antibiotics are usually the go-to solution, sometimes they just don’t do the trick.
UTI Statistics: A Closer Look
Did you know that about 60% of women will experience a UTI at some point in their lives? And let’s not forget men—they’re not completely off the hook either, though their risk is lower. But here’s the alarming part: up to 30% of UTIs don’t respond to standard antibiotic treatment, leading to persistent symptoms and frustration. So, why does this happen?
Why Does UTI Persist After Antibiotics?
There are several reasons why a UTI might stick around even after two rounds of antibiotics. Let’s break it down:
- Antibiotic Resistance: Bacteria can evolve and develop resistance to antibiotics, making them harder to kill.
- Incomplete Treatment: Sometimes, people stop taking antibiotics as soon as they feel better, which can allow some bacteria to survive and multiply.
- Complex UTIs: Some UTIs are more complicated than others, involving different types of bacteria or affecting different parts of the urinary tract.
- Underlying Health Conditions: Conditions like diabetes or a weakened immune system can make it harder for the body to fight off infections.
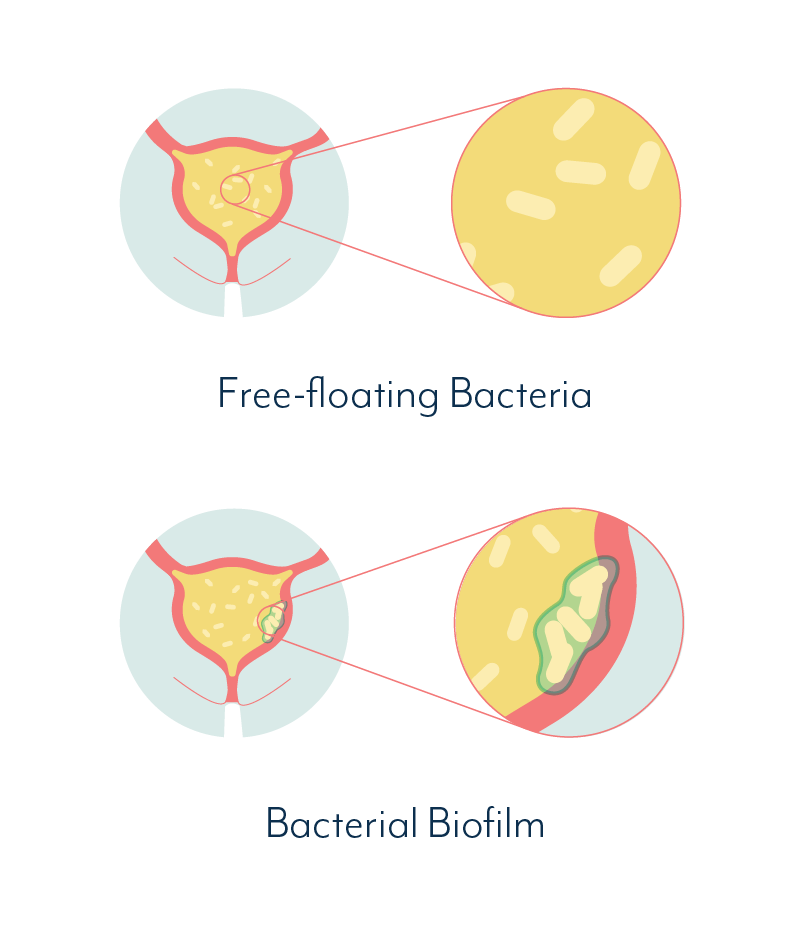
Think of it like a game of hide-and-seek. Some bacteria are really good at hiding, and antibiotics might not be able to reach them all. This can lead to a persistent infection that just won’t go away.
Common Mistakes People Make
One of the biggest mistakes people make is stopping their antibiotics early. I get it, you feel better, and you think, “I don’t need these anymore.” But here’s the thing: even if your symptoms disappear, there might still be bacteria lurking around. Always finish the full course of antibiotics, even if you start feeling better halfway through.
Read also:Update On Ami Brown The Rising Star In The Spotlight
Types of UTIs and Their Complexity
Not all UTIs are created equal. There are different types, and some are more complex than others. Let’s take a look:
- Cystitis: This is the most common type of UTI, affecting the bladder. It’s usually caused by E. coli and can be treated with antibiotics.
- Pyelonephritis: This is a kidney infection, which is more serious and requires immediate medical attention.
- Urethritis: This affects the urethra and is often caused by sexually transmitted infections (STIs).
Complex UTIs, on the other hand, might involve multiple types of bacteria or affect people with underlying health conditions. These can be trickier to treat and might require a more comprehensive approach.
Factors Contributing to Complex UTIs
Complex UTIs can be influenced by several factors, including:
- Poor immune function
- Structural abnormalities in the urinary tract
- Obstructions like kidney stones
- Previous UTIs that weren’t fully treated
Understanding the type of UTI you’re dealing with is crucial in determining the best course of action. That’s why it’s important to work closely with your healthcare provider.
Antibiotic Resistance: A Growing Concern
Antibiotic resistance is a big deal. It happens when bacteria evolve and develop ways to survive the effects of antibiotics. This can make infections harder to treat and can lead to longer illnesses, more doctor visits, and the need for stronger, more expensive drugs.
Here’s a scary stat: the World Health Organization (WHO) estimates that antibiotic resistance could cause 10 million deaths globally by 2050 if we don’t take action. That’s why it’s so important to use antibiotics responsibly and only when necessary.
Preventing Antibiotic Resistance
There are several steps you can take to prevent antibiotic resistance:
- Only take antibiotics when prescribed by a healthcare professional
- Always finish the full course of antibiotics, even if you feel better
- Avoid sharing antibiotics with others
- Practice good hygiene to prevent infections in the first place
Remember, antibiotics aren’t the answer to every health issue. Sometimes, your body can fight off infections on its own, and using antibiotics unnecessarily can do more harm than good.
The Diagnosis Process: What to Expect
If you suspect you have a UTI that won’t go away, it’s important to see a healthcare provider. They’ll likely perform a few tests to determine the cause of your symptoms:
- Urinalysis: This test checks for white blood cells, red blood cells, and bacteria in your urine.
- Urine Culture: This test identifies the specific type of bacteria causing the infection, which can help determine the best antibiotic to use.
- Imaging Tests: In some cases, your doctor might order an ultrasound or CT scan to check for structural abnormalities in your urinary tract.
Don’t be afraid to ask questions during your appointment. Understanding your diagnosis and treatment plan is key to taking control of your health.
Getting a Second Opinion
If you’re not satisfied with your initial diagnosis or treatment plan, don’t hesitate to get a second opinion. A different perspective can sometimes make all the difference, especially when dealing with persistent UTIs.
Alternative Treatments for Persistent UTIs
While antibiotics are the first line of defense against UTIs, there are alternative treatments that might help if they’re not working. Here are a few options:
- Cranberry Supplements: Some studies suggest that cranberry supplements can help prevent UTIs by preventing bacteria from sticking to the walls of the urinary tract.
- Probiotics: Probiotics can help restore the natural balance of bacteria in your body, which might reduce the risk of recurrent UTIs.
- Herbal Remedies: Certain herbs, like uva ursi and goldenseal, have been used traditionally to treat UTIs. However, always consult with a healthcare provider before trying herbal remedies.
Remember, alternative treatments should complement—not replace—conventional medical care. Always talk to your doctor before trying anything new.
Taking an Integrative Approach
Combining conventional and alternative treatments can sometimes yield the best results. For example, you might take antibiotics as prescribed by your doctor while also incorporating cranberry supplements and probiotics into your routine. This integrative approach can help address the infection from multiple angles.
Lifestyle Changes to Prevent Recurrence
Prevention is key when it comes to UTIs. Making a few lifestyle changes can significantly reduce your risk of recurrence:
- Stay Hydrated: Drinking plenty of water helps flush bacteria out of your urinary tract.
- Urinate After Intercourse: This can help clear any bacteria that might have been introduced during sex.
- Avoid Irritants: Certain products, like bubble baths and feminine hygiene sprays, can irritate your urinary tract and increase your risk of infection.
- Wear Breathable Underwear: Opt for cotton underwear and avoid tight-fitting clothes to keep the area dry and ventilated.
These small changes can make a big difference in the long run. And let’s be honest, who doesn’t want to avoid another round of antibiotics?
Dietary Tips for UTI Prevention
Your diet can also play a role in preventing UTIs. Here are a few tips:
- Drink cranberry juice (without added sugar)
- Increase your intake of probiotic-rich foods like yogurt and kefir
- Avoid caffeine and alcohol, which can irritate your bladder
- Include plenty of fruits and vegetables in your diet
Nutrition is a powerful tool in maintaining urinary tract health, so don’t underestimate its importance.
Home Remedies That Might Help
While home remedies aren’t a substitute for medical treatment, they can provide some relief from UTI symptoms:
- Heat Therapy: Applying a warm compress to your lower abdomen can help relieve pain and discomfort.
- Baking Soda: Adding baking soda to a glass of water can help neutralize the acid in your urine, reducing burning sensations.
- Stay Hydrated: Drinking plenty of water is one of the best things you can do for a UTI.
These remedies can help you feel better while you’re waiting for antibiotics to kick in or while exploring alternative treatments.
Finding Natural Relief
Natural remedies can be a great complement to medical treatment. Just remember to use them wisely and always consult with your healthcare provider before trying anything new.
:max_bytes(150000):strip_icc()/uti-symptoms-after-antibiotics-5186681_final-ccf49cce9177448cb225b4ef481b7a28.jpg)
